Abstract

Context: Prognosis of lower-risk (IPSS low/int-1) MDS is heterogeneous. Current prognostic systems rely on steady-state values for cytopenias. Capturing the dynamics of these parameters could yield additional prognostic information. We analyzed the prognostic relevance of relative drop (%) in neutrophil (ANC) and platelet (PLT) counts during the first six months follow-up of lower-risk MDS patients included in the EUMDS registry.
Methods: TheEUMDS registry includes prospectively patients (pts) within the first 100 days of diagnosis of lower-risk (IPSS low/intermediate-1) MDS. We performed a landmark analysis of overall survival (OS) in pts with a visit at 6±1 months from inclusion to assess the prognostic relevance of a relative drop in ANC and PLT over the first 6 months follow-up. Relative ANC and PLT drops were defined as: (ANC at landmark - ANC at inclusion) / ANC at inclusion, respectively (resp) for PLT.
Results: As of Sept 2016,1,800 patients with ≥5 months follow-up were included in the registry. 807 patients with a second visit at 6±1 months from inclusion were analyzed. Reasons for exclusion from this cohort were: no visit within the strict limits of 6±1 month (n=904), no PLT count at baseline (n=40) or 6-month visit (n=20), and no follow-up beyond 6-month visit (n=19). Median age was 73 yr, IPSS-R was very-low, low, intermediate or higher in 26%, 43% 24% and 7% of pts, resp. Median time to landmark was 183 days. Median follow-up from landmark was 37.8 months. Median relative drop in ANC and PLT was 5.2% and 4.6%, resp. At landmark, 41 patients (5%) received treatments affecting ANC or PLT (hypomethylating agents, lenalidomide or hydroxycarbamide). Excluding them did not affect results. Relative ANC and PLT drop were dichotomized at the 25% threshold. Sensitivity analyses with different cutoffs did not affect our final conclusions. Multivariate logistic regressions identified RBC- transfusion dependency (TD) at inclusion (OR=1.7, p=0.02) as the main predictor of 6-month relative PLT drop > 25%, while higher baseline ANC as a continuous value was associated with 6-month ANC drop >25% (10-4). The latter suggests that the dynamic range of ANC does not allow uniform assessment of ANC drop in all MDS patients.
In univariate analysis, a relative drop in PLT >25% (HR=2.3, p<10-4) was associated with shorter OS after the 6-month landmark (median 29.2 months vs 57.1 in pts with PLT drop ≤25%, p<10-4), and increased cumulative incidence of progression (CIP: standardized HR: 2.5, p<10-4), while relative ANC drop >25% only predicted higher CIP (standardized HR: 1.5, p=0.03), without significant impact on OS (p=0.12). The adverse prognosis of relative PLT drop was observed regardless of baseline IPSS-R or absolute PLT count at inclusion or landmark.
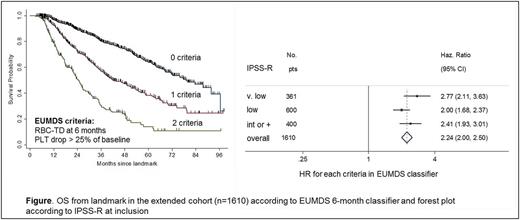
We subsequently divided our cohort in a training (n=403) and a validation (n=404) set to derive a prognostic model applicable at the 6-month landmark. Variables included age, gender and IPSS-R at inclusion, RBC-TD, steady-state PLT and ANC values at landmark, and relative PLT and ANC drop (with the 25% cutoff). Cox models with variable selection by penalized regression identified older age (p<10-4), RBC-TD at landmark (p<10-4) and relative PLT drop >25% (p=0.005) as independent prognostic factors. We built a simple age-independent 6-month EUMDS classifier based on RBC-TD at landmark and relative PLT drop >25%, where patients with none (53%), either (31%) or both criteria (16%) had median OS from landmark of 71, 42 and 19 months, resp, p<10-4). The classifier performed equally well in the validation set (p<10-4). A sensitivity analysis relaxing the timing of landmark drop was carried on an 'extended cohort' of 1610 (89%) registry pts with a second visit within ten months of inclusion. This analysis confirmed the adverse prognostic value of a relative PLT drop >25% within 10 months of diagnosis of lower-risk MDS and the broad applicability of the EUMDS classifier, regardless of baseline IPSS-R risk (Figure).
Conclusion: Early drop in platelets during the first 6 months of follow-up holds prognostic significance in lower-risk MDS. A 6-month classifier based on RBC-TD at 6 month and a relative platelet drop greater than 25% can inform prognosis of lower-risk MDS independently from IPSS-R.
Itzykson: Novartis: Research Funding; Janssen: Research Funding. Sanz: Gamida Cell: Research Funding. Germing: Janssen: Honoraria; Novartis: Honoraria, Research Funding; Celgene: Honoraria, Research Funding. Almeida: Novartis: Consultancy; Celgene: Consultancy; Bristol Meyer Squibb: Honoraria; Alexion: Honoraria; Servier: Consultancy. Fenaux: Astex: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Astex: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal